Share this post
What Causes Stress
Whether physical, mental, or emotional, stress stimulates a biological response that creates a chemical and hormonal surge throughout the body.[1] This response, known as the activation of the sympathetic nervous system (SNS), allows us to deal with the stressor by generating more strength to fight it or better cardiovascular output to run from it. After the reaction occurs, your body should relax and recover because while stress hormones can be a good and natural thing, frequent unrelenting stress can negatively affect your long-term physical and mental health. [2]
There are natural ways to reduce stress, which include easy diet and lifestyle changes. We’ll cover these and more in this guide. You can also download our free Stress Support Guide to reference at any time.
The 3 Stages of Stress
The stress response typically occurs in three phases[3]:
- Alarm stage – This is where we feel the initial symptoms of stress or the “fight-or-flight” response. The heart rate increases, the adrenal glands release cortisol and adrenaline, and there’s a boost of anxious energy.
- Resistance stage – After the shock and initial reaction to a stressor, the body begins to normalize. The heart rate and blood pressure start to normalize, and cortisol is released in lower amounts. Though the body is trying to recover, it does so slowly to remain on high alert and return to stage one if needed. If the stressor subsides, then the body will return to homeostasis. If the stressful situation continues, your body continues to elicit a physical and hormonal stress response.
- Exhaustion stage – If stress becomes chronic or prolonged, our body continues to experience the physical effects. Remaining in this state for extended periods can drain your physical, mental, and emotional resources until you feel burnt out or exhausted. The physical effects of this stage leave you at higher risk for stress-related illnesses, such as a weakened immune system, chronic anxiety, cardiovascular disease, gastrointestinal issues, metabolic dysfunction, and more, with additional negative effects on mental health.
The Stress-Cortisol Connection
Cortisol is a necessary hormone that has many benefits for us as the primary glucocorticoid we produce. It’s when stress becomes chronic and cortisol elevations are excessive that it can cause problems. [4] When released, it increases blood sugar levels by inducing the production of additional glucose molecules via gluconeogenesis. [5] It also alters our metabolism to support the nutrient requirements of our nervous system during stress. [6] It constricts blood vessels to increase blood pressure. [7] It modulates our inflammation response by reducing inflammatory cytokines and histamines. [8] It temporarily boosts our energy and resilience. Each of these effects helps us deal with acute stressors or dangers we may encounter, yet it’s easy to see how they can become problematic if maintained over a long time. Chronic stress can affect almost every single organ system in our body.
Stress and the GI System
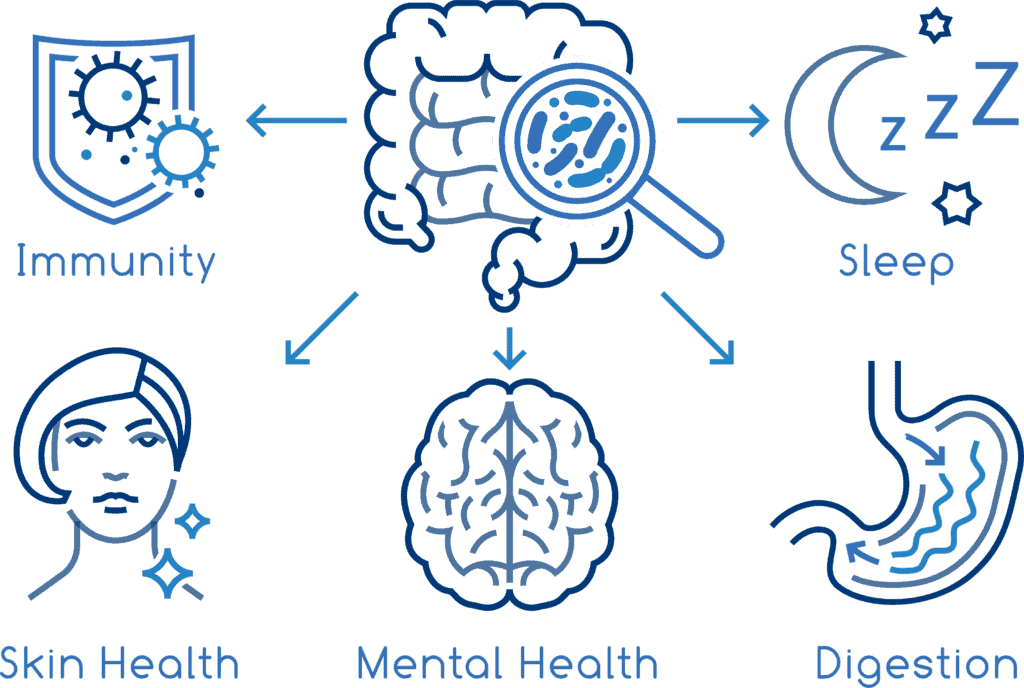
The brain and the gut are constantly in communication. These two centers have bi-directional communication, with each being able to impact the other. [9] Because of this, stress can directly affect gut function in multiple ways.
Stress can alter the way our entire gastrointestinal system functions and alter our digestion. [10] For example, SNS activation suppresses gastric acid secretion while adjusting the speed of digestion throughout the tract. [11] During stress, transit times will increase in the colon while slowing down in the small intestine. [12] These changes are how our body prioritizes dealing with our stressors before digestion. By halting the breakdown of food, we won’t have to stop and use the restroom when we need to escape or fight instead.
How Stress Affects the Gut
These changes not only affect the speed at which we digest but can have long-term impacts on the function of digestion through our microbiome, or the bacteria living in our gut. For instance, a decrease in gastric acid secretion can create a higher pH, giving rise to a suitable environment for opportunistic, pathological bacteria growth. [13] Alterations in transit time alter the distribution of gut microbes, as areas of slower transit time lead to more fermentation and bacterial growth, where areas of faster transit time have less. [14]
These changes help explain why stressful situations are associated with a proinflammatory gut environment and a reduction in microbiome diversity. [15] There are also additional factors, such as how stress can negatively impact diet. Diets rich in sugars, saturated fats, and processed foods tend to breed lower microbial diversity and greater instances of leaky gut. [16] Alternatively, diets high in fiber, plant protein, and unsaturated fats support a healthy, diverse microbiome. 17
Stress and the Gut Brain Axis
To add insult to injury, changes in the microbiome and gut function can exacerbate stress through the gut-brain axis. Yes, stress and mental health can be worsened by the gut dysfunction it initially caused. Microbes can produce neurochemicals and hormones that are identical to ours that go on to cross the intestinal barrier and elicit change. [17] The gut microbiota can also regulate many of our critical neurotransmitters by altering the levels of their precursors. [18] For example, Bifidobacterium infantas can elevate plasma tryptophan levels, a precursor to serotonin. [19] Studies have even shown that specific probiotic strains that produce certain neurotransmitters can boost the concentration of those neurotransmitters in our bodies. [20] These studies have led to some novel research in the world of psychobiotics, defined as live organisms that produce health benefits in patients suffering from psychiatric illness when ingested in adequate amounts. [21]
Stress and Sleep
Stress and lack of sleep don’t mix. The same HPA axis that stimulates our stress hormones is also responsible for regulating our sleep. Chronic stress disrupts the HPA axis, as well as our sleep cycles making it difficult to fall asleep.[22] Our stress hormones like cortisol and norepinephrine induce an arousing effect that keeps us alert, even when we prefer to sleep. [23] This heightened state of arousal can delay the onset of sleep and give rise to anxious thoughts that further exacerbate insomnia.
Many of us who have experienced stress-induced insomnia know that it’s hard to get good sleep when we’re stressed, but that sleep is often just what we need. Better sleep helps us manage stress by calming the HPA axis and the SNS, while restless sleep increases cortisol and norepinephrine. [24] These results can be cumulative, meaning that creating poor sleep habits over time can lead to even more hormonal dysfunction, predisposing us to an unhealthy stress response. [25]
How to Improve Sleep Quality to Reduce Stress
We can do things to combat poor sleep quality, even when our stress levels make snoozing difficult. It’s essential to practice good sleep hygiene and initiate methods that support a healthy circadian rhythm.[26] Some examples are:
- Make a cool, dark, comfortable environment in your sleep space
- Turn off all electronics one hour before bed
- Avoid caffeine later in the day
- Avoid alcohol before bed
- Create a routine or pattern, sleeping at the same time each day
Stress and Sexual Health
Our SNS prioritizes essential processes and actively diminishes functions that are considered non-essential during a stressor.[27] Sex and libido, unfortunately, fall into this category. When stress levels remain high, the body repurposes the building blocks of our stress hormones to build more cortisol, leading to a decrease in the hormones responsible for our sex drive.[28] Testosterone, progesterone, and estrogen levels can all be negatively affected during times of stress.[29]
Cortisol also narrows arteries and restricts blood flow to the unnecessary organs, like the genitals, during stressful situations. Blood flow to the pelvis is instrumental for arousal. [30] These physiological changes are, of course, in addition to the mental strain that comes with stress, which often serves as a distraction from sexual desire.
Stress and the Thyroid
Cortisol slows our metabolism to prioritize fighting stressors, and that includes the production of our thyroid hormones.[31] Cortisol suppresses HPA axis function, including the pituitary gland, where we make thyroid-stimulating hormone (TSH). Because of this, our thyroid function slows, leading to less overall production of triiodothyronine (T3) and thyroxine (T4), our thyroid hormones.[32] Additionally, stress slows the conversion of T4 to the biologically active T3, leading to an increase in hypothyroid symptoms and higher levels of reverse T3.
Stress also strongly correlates with incidences of autoimmune thyroid disorders, such as Grave’s disease and Hashimoto’s thyroiditis. [33] Under normal conditions, cortisol modulates the immune system and can have beneficial effects on autoimmune diseases. However, in times of chronic stress, cortisol fluctuations can trigger multiple autoimmune disorders, with autoimmune thyroid disorders having a strong association.[34]
Stress and the Immune System
Our immune system responds to signals from both the nervous and endocrine systems, and therefore is vulnerable to stress-related change.[35] During acute stress, our body adapts to either run or fight something dangerous. For the immune system, this means an upregulation of our innate immune system by redistributing the blood cells to be ready for a possible injury or infection. In contrast, our specific immune response, or second-line immune defense against non-self pathogens, is downregulated during times of acute stress.[36] The specific immune response involves more significant energy needs and is de-prioritized in acute stress.36
In periods of chronic stress, the immune system is globally suppressed. Chronic stress is associated with decreases in natural killer cells, lymphocytes, gamma interferon, and the T cell response.[37] This response leaves the stressed individual more susceptible to infections.[38] Additionally, chronic stress is correlated with higher incidences of autoimmune disease and some cancers due to the associated immune changes.34
How To Reduce Stress
Follow the tips below for easy ways to help reduce stress. You can also download our free stress support guide.
Exercise to Reduce Stress and Anxiety
Exercising regularly has been shown to help manage stress and its physical effect on the body, while improving overall mental health.[39],[40] There are several proposed mechanisms by which physical movement can aid in stress management. Physically fit individuals exhibit a lower activation of the physiological stress response when a stressor is administered.[41] This could be because exercise stimulates the HPA axis and triggers a cortisol release. Repeated exposure to a particular stressor, in this case, exercise, can result in HPA axis adaptation, meaning the HPA axis becomes trained to have a milder stress response.[42]
Studies have shown that regular exercisers demonstrate adaptations of the HPA axis and decreased peripheral sensitivity to glucocorticoids like cortisol.[43] Studies show that regular exercise also reduces circulating cortisol levels in the body.[44]
Learning how to add exercise into your day may also boost endorphin, or feel-good neurotransmitter, production to up to 5x the basal serum concentrations.[45] Increased concentrations of these endorphins can directly improve mood and mental wellbeing, but they can also have effects on our other stress hormones. Higher levels of circulating endorphins have been shown to suppress levels of adrenocorticotropic hormone (ACTH) and cortisol.[46] Many forms of exercise show benefit, from yoga[47] to weightlifting[48], so choose an activity that’s enjoyable to you and incorporate it into your daily routine.
Try Deep Breathing
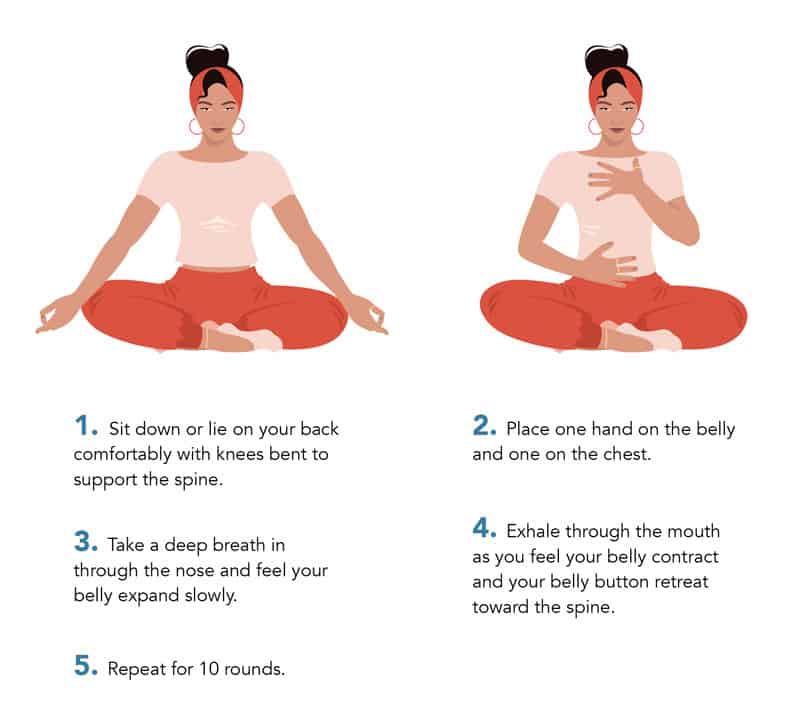
Deep breathing has been shown to modulate the autonomic nervous system and help shift the body from a sympathetic, or fight or flight, state into a parasympathetic state, making it a valuable tool to combat stress. [49] Studies have shown that relaxation techniques like deep breathing can reduce our heart rate and salivary cortisol levels while providing effective stress relief. [50] When you’re feeling overwhelmed, pause and take ten seconds to breathe.
Follow the steps below to easily incorporate deep breathing into your day:
Nutrients and Supplements for Stress Support
 B Vitamins for Stress
B Vitamins for Stress
B vitamins are important cofactors that are necessary to make our neurotransmitters as well as support almost every metabolic process in the body.[64] They have been shown to benefit parameters of stress and mood. [65] One reason B vitamins can help relieve stress and anxiety is their role in the methylation cycle. Our methylation cycle depends on vitamin B6, folate (B9), and B12 to recycle homocysteine, a harmful amino acid, into methionine.[66] High levels of homocysteine have been associated with poor cognitive function and negative mood, among other issues.66 B vitamins can be found in leafy greens, fatty fish, eggs, organ meats, and legumes, though those who lack a balanced healthy diet might benefit from supplementation.
How GABA Reduces Stress
GABA is an inhibitory neurotransmitter, meaning it mediates or turns down the neurotransmitters associated
 L-theanine for Relaxation
L-theanine for Relaxation
One of the predominant ingredients in green tea, L-theanine can be a great option during times of stress and anxiety. L-theanine is an amino acid that increases alpha-wave activity in the brain, much like GABA.[69] Supplementation with L-theanine can have a relaxing effect, reducing anxiety and providing some stress reduction. [70] Studies suggest that L-theanine could also increase serotonin and dopamine levels. [71]
Adaptogens to Reduce Stress
Adaptogens are herbs that improve an individual’s ability to cope with stress, initially defined as enhancing the “state of non-specific resistance.”[51] These herbs are a class of metabolic regulators that protect against stress-related damage to the system by helping an individual adapt to their current conditions. Many of them have direct actions on cortisol and the HPA axis, while also acting as anxiolytics to reduce the mental effects of stress.[52] Some adaptogens even increase mental work capacity, often diminished in times of stress, to expand an individual’s tolerance to mental exhaustion.[53] Adaptogens are not only a useful tool when it comes to regulating the hormonal dysfunction associated with stress, but also for direct stress relief.
For an herb to be classified as an adaptogen, it must reduce stress-induced damage and present stress-protective effects such as anti-fatigue, immune-protective, and/or restorative properties. An adaptogen should exhibit stimulating effects and increase working capacity in times of fatigue and stress, yet they must not deplete energetic resources or cause negative side effects. They must be innocuous and not disrupt the body’s natural state, only exerting a normalizing effect on pathological states.50
Adaptogens are not meant to just lower cortisol across the board, but rather to support the ideal circadian rhythm. And while substances classified as adaptogens may have these qualities in common, they also have individual qualities that make them unique and ideal for certain situations. Some of our favorite adaptogens for mental wellbeing include:
Magnolia officinalis (Magnolia)
Magnolia bark has a long history of use in traditional Chinese medicine 
Withania somnifera (Ashwagandha)
Ashwagandha root has a long history of use in ayurvedic medicine. Ancient documents claim its benefits for “rejuvenating the system” and “improving lifespan”.[56] 
Rhodiola rosea (Rhodiola)
Rhodiola is an energizing adaptogen that is often used in cases of fatigue resulting from chronic stress.[58] It has been shown to reduce anxiety levels while improving energy. Rhodiola also enhances cognition and has been shown to improve parameters of memory and brain fog resulting from stress.[59]
Melissa officinalis (Lemon balm)
Lemon balm has a long history of use for stress relief. It inhibits the 
 Matricaria recutita (German chamomile)
Matricaria recutita (German chamomile)
More than just a bedtime tea, chamomile is well-known for its anxiolytic, calming effects. It has been shown to help modulate the cortisol response under acute stress and reduce cortisol levels significantly in times of chronic stress. [63]
Download Our Free Stress Support Guide
 References
References
Click here to see References
[1] Keller J, et al. HPA axis in major depression: cortisol, clinical symptomatology and genetic variation predict cognition. Molecular Psychiatry. 2017;22(4):527-36.
[2] Adam EK, et al. Diurnal cortisol slopes and mental and physical health outcomes: A systematic review and meta-analysis. Psychoneuroendocrinology. 2017;83:25-41.
[3] SELYE H. Stress and the general adaptation syndrome. Br Med J. 1950;1(4667):1383-1392.
[4] Finnerty CC, et al. The surgically induced stress response. JPEN. 2013 Sep;37(5 Suppl):21S-9S.
[5] Hackett RA, Steptoe A. Type 2 diabetes mellitus and psychological stress – a modifiable risk factor. Nat Rev Endocrinol. 2017;13(9):547-560. doi:10.1038/nrendo.2017.64
[6] Epel ES, et al. Stress may add bite to appetite in women: a laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology. 2001;26:37-49.
[7] Liu MY, Li N, Li WA, Khan H. Association between psychosocial stress and hypertension: a systematic review and meta-analysis. Neurol Res. 2017;39(6):573-580. doi:10.1080/01616412.2017.1317904
[8] Steptoe A, et al. The effects of acute psychological stress on circulating inflammatory factors in humans: A review and meta-analysis. Brain, Behavior, and Immunity. 2007;21:901-12.
[9] Mackos AR, Maltz R, Bailey MT. The role of the commensal microbiota in adaptive and maladaptive stressor-induced immunomodulation. Horm Behav. 2017;88:70-78. doi:10.1016/j.yhbeh.2016.10.006
[10] Huang EY, Inoue T, Leone VA, et al. Using corticosteroids to reshape the gut microbiome: implications for inflammatory bowel diseases. Inflamm Bowel Dis. 2015;21(5):963-972. doi:10.1097/MIB.0000000000000332
[11] Yang, H., Yuan, P.Q., Wang, L., Tache, Y., 2000. Activation of the parapyramidal region in the vetral medulla stimulates gastric acid secretion through vagal pathways in rats. Neuroscience 95, 773-779
[12] Zhao, X., Yin, J., Wang, L., Chen, J.D., 2014. Diffused and sustained inhibitory effects of intestinal electrical stimulation on intestinal motility mediated via sympathetic pathway. Neuromodulation : journal of the International Neuromodulation Society 17, 373-379; discussion 380.
[13] Galley JD, Bailey MT. Impact of stressor exposure on the interplay between commensal microbiota and host inflammation. Gut Microbes. 2014;5(3):390-396. doi:10.4161/gmic.28683
[14] Tache, Y., Martinez, V., Million, M., Wang, L., 2001. Stress and the gastrointestinal tract III. Stress-related alterations of gut motor function: role of brain corticotropin-releasing factor receptors. . American journal of physiology. Gastrointestinal and liver physiology 280, G173- G177.
[15] Lyte M, Ernst S. Catecholamine induced growth of gram negative bacteria. Life Sci. 1992;50(3):203-212. doi:10.1016/0024-3205(92)90273-r
[16] Corrêa-Oliveira R, Fachi JL, Vieira A, Sato FT, Vinolo MA. Regulation of immune cell function by short-chain fatty acids. Clin Transl Immunology. 2016;5(4):e73. Published 2016 Apr 22. doi:10.1038/cti.2016.17
[17] Lyte M, Ernst S. Alpha and beta adrenergic receptor involvement in catecholamine-induced growth of gram-negative bacteria. Biochem Biophys Res Commun 190: 447–452, 1993. doi:10.1006/bbrc.1993.1068.
[18] Dinan TG, Cryan JF. The Microbiome-Gut-Brain Axis in Health and Disease. Gastroenterol Clin North Am. 2017;46(1):77-89. doi:10.1016/j.gtc.2016.09.007
[19] . Desbonnet L, Garrett L, Clarke G, et al. Effects of the probiotic Bifidobacterium
infantis in the maternal separation model of depression. Neuroscience 2010;
170(4):1179–88
[20] . Lyte M. Microbial endocrinology in the microbiome-gut-brain axis: how bacterial production and utilization of neurochemicals influence behavior. PLoS Pathog 2013;9(11):e1003726
[21] Dinan TG, Stanton C, Cryan JF. Psychobiotics: a novel class of psychotropic. Biol Psychiatry. 2013;74(10):720-726. doi:10.1016/j.biopsych.2013.05.001
[22] Kalmbach DA, et al. The impact of stress on sleep: Pathogenic sleep reactivity as a vulnerability to insomnia and circadian disorders. J Sleep Res. 2018;27(6):e12710.
[23] Fernandez-Mendoza J, Vgontzas AN. Insomnia and its impact on physical and mental health. Curr Psychiatry Rep. 2013;15(12):418. doi:10.1007/s11920-013-0418-8
[24] Vgontzas AN, Tsigos C, Bixler EO, et al. Chronic insomnia and activity of the stress system: a preliminary study. J Psychosom Res. 1998;45(1):21-31. doi:10.1016/s0022-3999(97)00302-4
[25] Vgontzas AN, Bixler EO, Lin HM, Prolo P, Mastorakos G, Vela-Bueno A, et al. Chronic insomnia is associated with nyctohemeral activation of the hypothalamic-pituitary-adrenal axis: clinical implications. J Clin Endocrinol Metab. 2001;86:3787–3794
[26] Irish LA, et al. The role of sleep hygiene in promoting public health: A review of empirical evidence. Sleep Med Rev. 2015;22:23-36.
[27] Jiang W, Zhang XZ, Gu ML. Zhonghua Yi Xue Yi Chuan Xue Za Zhi. 2013;30(5):565-569. doi:10.3760/cma.j.issn.1003-9406.2013.05.012
[28] Handa RJ, Weiser MJ. Gonadal steroid hormones and the hypothalamo-pituitary-adrenal axis. Front Neuroendocrinol. 2014;35(2):197-220. doi:10.1016/j.yfrne.2013.11.001
[29] Heck AL, et al. Sex differences in the hypothalamic-pituitary-adrenal axis’ response to stress: an important role for gonadal hormones. Neuropsychopharmacology. 2019;44(1):45-58.
[30] Szewczyk, Katarzyna, and Christian Zidorn. “Ethnobotany, phytochemistry, and bioactivity of the genus Turnera (Passifloraceae) with a focus on damiana–Turnera diffusa.” Journal of ethnopharmacology vol. 152,3 (2014): 424-43. doi:10.1016/j.jep.2014.01.019
[31] Liyanarachchi K, Ross R, Debono M. Human studies on hypothalamo-pituitary-adrenal (HPA) axis. Best Pract Res Clin Endocrinol Metab. 2017;31(5):459-473. doi:10.1016/j.beem.2017.10.011
[32] Walter, K.N., Corwin, E.J., Ulbrecht, J. et al. Elevated thyroid stimulating hormone is associated with elevated cortisol in healthy young men and women. Thyroid Res 5, 13 (2012).
[33] Tsatsoulis A. The role of stress in the clinical expression of thyroid autoimmunity. Ann N Y Acad Sci. 2006;1088:382-395. doi:10.1196/annals.1366.015
[34] Stojanovich L, Marisavljevich D. Stress as a trigger of autoimmune disease. Autoimmun Rev. 2008;7(3):209-213. doi:10.1016/j.autrev.2007.11.007
[35] Vitlic A, Lord JM, Phillips AC. Stress, ageing and their influence on functional, cellular and molecular aspects of the immune system. Age (Dordr). 2014;36(3):9631.
[36] Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull. 2004;130(4):601-630.
[37] Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull. 2004;130(4):601-630.
[38] Ben-Eliyahu S, Shakhar G, Page GG, Stefanski V, Shakhar K. Suppression of NK cell activity and of resistance to metastasis by stress: a role for adrenal catecholamines and beta-adrenoceptors. Neuroimmunomodulation. 2000;8(3):154-164. doi:10.1159/000054276
[39] Seaward BL. Physical exercise: Flushing out the stress hormones. In: Essentials of Managing Stress. 4th ed. Jones & Bartlett Publishers; 2017.
[40] Physical Activity Guidelines for Americans. 2nd ed. U.S. Department of Health and Human Services. https://health.gov/our-work/physical-activity/current-guidelines. Accessed Aug. 10, 2020.
[41] Pedersen, B. K., & Saltin, B. (2015). Exercise as medicine – evidence for prescribing exercise as therapy in 26 different chronic diseases. Scandinavian Journal of Medicine & Science in Sports, 25, 1–72. doi:10.1111/sms.12581
[42] Wittert GA, Livesey JH, Espiner EA, Donald RA. Adaptation of the hypothalamopituitary adrenal axis to chronic exercise stress in humans. Med Sci Sports Exerc. 1996;28(8):1015-1019. doi:10.1097/00005768-199608000-00011
[43] Duclos M, Tabarin A. Exercise and the Hypothalamo-Pituitary-Adrenal Axis. Front Horm Res. 2016;47:12-26. doi:10.1159/000445149
[44] Beserra AHN, Kameda P, Deslandes AC, Schuch FB, Laks J, Moraes HS. Can physical exercise modulate cortisol level in subjects with depression? A systematic review and meta-analysis. Trends Psychiatry Psychother. 2018;40(4):360-368. doi:10.1590/2237-6089-2017-0155
[45] Working out boosts brain health. American Psychological Association. https://www.apa.org/topics/exercise-stress. Accessed Aug. 10, 2020.
[46] Harber VJ, Sutton JR. Endorphins and exercise. Sports Med. 1984;1(2):154-171. doi:10.2165/00007256-198401020-00004
[47] Pascoe MC, Thompson DR, Ski CF. Yoga, mindfulness-based stress reduction and stress-related physiological measures: A meta-analysis. Psychoneuroendocrinology. 2017;86:152-168. doi:10.1016/j.psyneuen.2017.08.008
[48] Oeland AM, Laessoe U, Olesen AV, Munk-Jørgensen P. Impact of exercise on patients with depression and anxiety. Nord J Psychiatry. 2010;64(3):210-217. doi:10.3109/08039480903511373
[49] Jerath R, Crawford MW, Barnes VA, Harden K. Self-regulation of breathing as a primary treatment for anxiety. Appl Psychophysiol Biofeedback. 2015;40(2):107-115. doi:10.1007/s10484-015-9279-8
[50] Perciavalle V, Blandini M, Fecarotta P, et al. The role of deep breathing on stress. Neurol Sci. 2017;38(3):451-458. doi:10.1007/s10072-016-2790-8
[51] Panossian A, Wikman G. Effects of Adaptogens on the Central Nervous System and the Molecular Mechanisms Associated with Their Stress-Protective Activity. Pharmaceuticals (Basel, Switzerland). 2010 Jan 19;3(1):188-224.
[52] Provino R. The role of adaptogens in stress management. Aust J Med Herbal. 2010;22:41-9.
[53] Panossian A, Wikman G. Evidence-based efficacy of adaptogens in fatigue, and molecular mechanisms related to their stress-protective activity. Current Clinical Pharmacology. 2009;4(3):198-219.
[54] Sarrica, Andrea et al. “Safety and Toxicology of Magnolol and Honokiol.” Planta medica vol. 84,16 (2018): 1151-1164. doi:10.1055/a-0642-1966
[55] Talbott SM, et al. Effect of Magnolia officinalis and Phellodendron amurense (Relora®) on cortisol and psychological mood state in moderately stressed subjects. Journal of the International Society of Sports Nutrition. 2013 Aug 7;10(1):37.
[56] Singh N, et al. An overview on ashwagandha: a Rasayana (rejuvenator) of Ayurveda. African Journal of Traditional, Complementary, and Alternative Medicines. 2011;8(5 Suppl):208-13.
[57] Candelario M, et al. Direct evidence for GABAergic activity of Withania somnifera on mammalian ionotropic GABAA and GABArho receptors. Journal of Ethnopharmacology. 2015;171:264-72.
[58] Panossian A, Wikman G, Sarris J. Rosenroot (Rhodiola rosea): traditional use, chemical composition, pharmacology and clinical efficacy. Phytomedicine. 2010;17(7):481-493.
[59] Tao H,et al. Rhodiola species: A comprehensive review of traditional use, phytochemistry, pharmacology, toxicity, and clinical study. Med Res Rev. 2019;39(5):1779-1850.
[60] Ibarra A, et al. Effects of chronic administration of Melissa officinalis L. extract on anxiety-like reactivity and on circadian and exploratory activities in mice. Phytomedicine. 2010;17:397-403.
[61] Taiwo AE, et al. Anxiolytic and antidepressant-like effects of Melissa officinalis (lemon balm) extract in rats: Influence of administration and gender. Indian J Pharmacol. 2012;44:189-92.
[62] Scholey A, et al. Anti-stress effects of lemon balm-containing foods. Nutrients. 2014 Oct 30;6(11):4805-21.
[63] Amsterdam, Jay D et al. Putative Antidepressant Effect of Chamomile (Matricaria chamomilla L.) Oral Extract in Subjects with Comorbid Generalized Anxiety Disorder and Depression. Journal of alternative and complementary medicine. 2020; (26)9
[64] Kennedy DO. B Vitamins and the Brain: Mechanisms, Dose and Efficacy–A Review. Nutrients. 2016;8(2):68. Published 2016 Jan 27.
[65] Young LM, Pipingas A, White DJ, Gauci S, Scholey A. A Systematic Review and Meta-Analysis of B Vitamin Supplementation on Depressive Symptoms, Anxiety, and Stress: Effects on Healthy and ‘At-Risk’ Individuals. Nutrients. 2019;11(9):2232. Published 2019 Sep 16. doi:10.3390/nu11092232
[66] Ash M. Review of homocysteine [Internet]. Clinical education; 2017 March 8 [cited 2018 Dec 19]. Available from: https://www.clinicaleducation.org/resources/reviews/review-of-homocysteine/
[67] Abdou AM, Higashiguchi S, Horie K, et al. Relaxation and immunity enhancement effects of gamma-aminobutyric acid (GABA) administration in humans. Biofactors. 2006;26(3):201-8.
[68] Petroff OA. GABA and glutamate in the human brain. Neuroscientist. 2002 Dec;8(6):562-73.
[69] Nobre AC, et al. L-theanine, a natural constituent in tea, and its effect on mental state. Asia Pac J Clin Nutr. 2008;17 Suppl 1:167-8.
[70] Nathan PJ, Lu K, Gray M, Oliver C. The neuropharmacology of L-theanine(N-ethyl-L-glutamine): a possible neuroprotective and cognitive enhancing agent. J Herb Pharmacother. 2006;6(2):21-30
[71] Wakabayashi C, Numakawa T, Ninomiya M, et al. Behavioral and molecular evidence for psychotropic effects in L-theanine. Psychopharmacology (Berl). 2012;219(4):1099-109.
The information provided is for educational purposes only. Consult your physician or healthcare provider if you have specific questions before instituting any changes in your daily lifestyle including changes in diet, exercise, and supplement use.
Share this post
Meagan Purdy
Related posts
The Benefits of Berry Polyphenols
The abundant polyphenols found in berries deliver numerous health benefits Of all fruits, the consumption of fresh berries is something we oft seek out more than their somewhat more boring apple or banana counterparts. Whether it be berry smoothies; berry cobblers, pies, or crisps; homemade berry wines; or simply fresh berries eaten by the…
Stimulants and Sedatives: The Good, the Bad, and the Ugly
Use now, pay later? Problems associated with common stimulants and sedatives In our go-go-go world, it’s easy to feel drawn to stimulant substances to keep us going and sedatives to help us relax. Whether it’s coffee to get through the day and a glass of wine after work, or medications such as methylphenidates or…
Shining Light on Seasonal Depression
Natural approaches to overcoming seasonal affective disorder (SAD) As charming as I found the quad of the University in the summer, the winter semesters at my alma mater were brutal. It was cold. It was dark. It was damp. Many of my classmates looked ashen, tired, and miserable. In those dark Canadian winters I…
Stress and Psychological Resilience
How the ability to “bounce back” affects our overall well-being Whether you have consciously thought of it or not, in the last months you have inevitably demonstrated some aspects of emotional and psychological resilience out of sheer necessity. In February of 2020, nary a handful of us anticipated the blows which March of 2020…
Alcohol and Tylenol Can Be a Deadly Combination
Why taking acetaminophen (paracetamol) for a hangover is a dangerous idea. The over-the-counter pain medication acetaminophen is a surprisingly controversial drug. Sold under the brand name Tylenol in North America and known as paracetamol in other countries, acetaminophen can be taxing to the liver. Acetaminophen is the number one cause of acute liver failure…
Vitamin C for Mood and Addiction
How ascorbic acid soothes the brain Beyond immune support Vitamin C (ascorbic acid) is best known for its immune-enhancing effects – from reducing the severity and duration of the common cold,[1] to supporting the health of individuals with HIV/AIDS,[2] to reducing the histamine response seen in allergies and asthma,[3],[4],[5] to even potentially reducing the…
Categories
- Botanicals (56)
- GI Health (53)
- Healthy Aging (121)
- Immune Support (39)
- In The News (39)
- Kids Health (21)
- Stress and Relaxation (50)
- Uncategorized (1)
- Video (9)
- Vitamins & Minerals (51)




 B Vitamins for Stress
B Vitamins for Stress L-theanine for Relaxation
L-theanine for Relaxation

 Matricaria recutita (German chamomile)
Matricaria recutita (German chamomile)

