Share this post
Where there’s a buck to be made…
With rapidly increasing rates of obesity and metabolic syndrome, nonalcoholic fatty liver disease (NAFLD) has become the most common causes of chronic liver disease in Western countries.[1] NAFLD affects 10 to 46% of the United States population, with a worldwide prevalence of 6 to 35%.[2] Actual numbers, of course, may be higher due to the silent nature of this metabolic syndrome companion. This trend has not gone unnoticed by those in the drug development market. Where there is a disease to treat, there is a buck to be made.
NAFLD affects 10 to 46% of the United States population, with a worldwide prevalence of 6 to 35%.
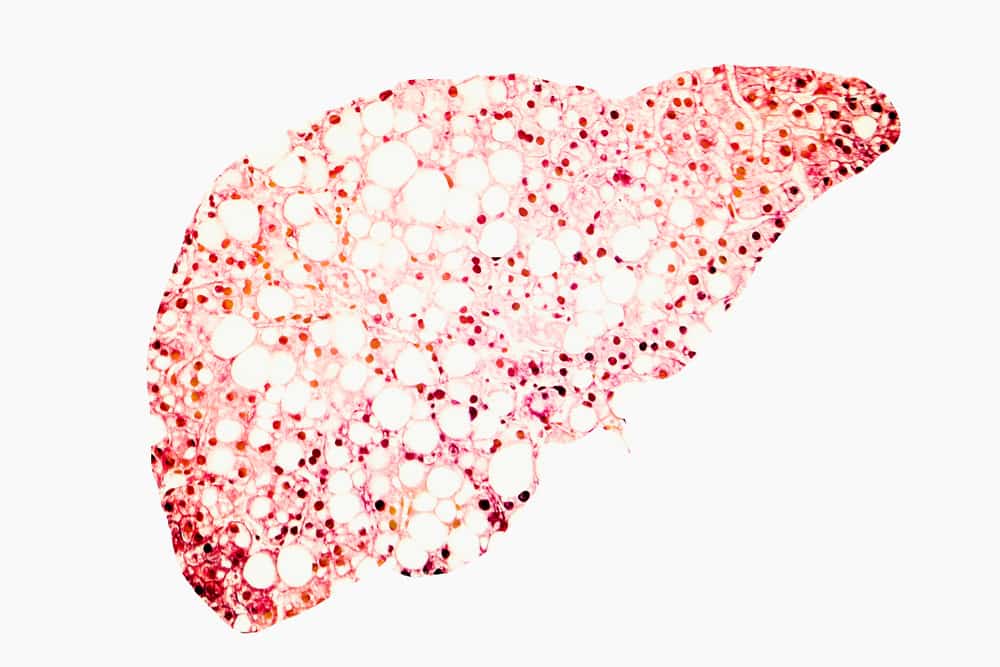
NAFLD is subdivided into nonalcoholic fatty liver (NAFL), liver fat accumulation without significant inflammation, and nonalcoholic steatohepatitis (NASH), fatty liver changes with inflammation (and cellular death). NAFL and NASH are considered “silent” diseases since they do not cause symptoms that would be noticed in a physician’s office without special tests. Although liver function tests (LFTs) are a part of the comprehensive metabolic panel (CMP) which many physicians routinely assess after age 50, this profile is often not performed unless there is a problem related to the liver that had presented when the patient was younger. Thus, the tissue changes and low level inflammatory state of NAFLD can go undiagnosed for many years and may even progress into hepatic cirrhosis, no different than that of end stage liver disease associated with alcoholism or chronic viral hepatitis. Unfortunately, even children are now being found to have NAFLD at an alarming rate – further giving reason we should have increased screening.[3]
Stages of liver disease: Normal healthy liver, fatty liver changes (NAFLD), fatty changes with inflammation (NASH), and cirrhosis (end-stage disease)
If LFTs are assessed, many physicians pass off mild elevations in alanine aminotransferase (ALT), aspartate aminotransferase (AST), and gamma-glutamyl transferase (GGT) as “normal” without further screening, particularly in individuals who are overweight or obese. Even when physicians take the extra steps to rule out infectious hepatitis and gallbladder-related disease, the only recommendations typically suggested that may impact elevated liver enzymes (attributed to NAFLD) are alcohol abstinence, weight loss, and the proper medical management of blood sugar and cholesterol, as there currently is no standard pharmaceutical treatment for NAFLD.[4]
Once a medication specifically for treating NAFLD is available, it won’t take long for both physicians and patients to be made aware of it, and increased screening will follow. Fortunately, there are ways to support liver health through nutrition, without having to rely on Big Pharma or wait for a “miracle drug”. In this article we will review the effects of antioxidants, botanicals, and probiotics on liver health.
Nutritional support for fatty liver disease
A prolonged state of oxidative stress and inflammation injures the cells of the liver and precedes the development of overt disease and scarring, which is an irreversible process. This is true for both alcoholic and nonalcoholic causes of liver disease. Thus, it is important to intervene and manage the earliest stages of the process, because the progression to NASH increases the risk of cirrhosis, liver failure, and hepatocellular carcinoma (liver cancer).
A variety of nutritional interventions have been shown to reduce liver inflammation and oxidative stress. Antioxidants are one thing that has been shown to improve outcomes in individuals with NAFLD.[5],[6] Glutathione is the primary antioxidant in the body and is of particular importance to liver health and function.[7] N-acetylcysteine, an antioxidant that provides the cysteine necessary for glutathione production, and other antioxidants such as lipoic acid and vitamins C and E all support levels of glutathione in the liver.[8],[9],[10] Lipoic acid also helps to improve blood sugar levels, an important consideration for individuals with metabolic syndrome.
Glutathione is the primary antioxidant in the body and is of particular importance to liver health and function. Antioxidants such as N-acetylcysteine, lipoic acid, and vitamins C and E all support levels of glutathione in the liver.
Phosphatidylcholine (PC), a primary component of lecithin, has been shown to protect against fibrosis (the thickening and scarring of tissue) associated with hepatitis.[11],[12] PC is a normal constituent of bile (which is produced in the liver and stored in the gallbladder) and facilitates the proper digestion of fats. Studies have shown that the dietary requirements for choline may be higher than previously anticipated, and that current average intakes may not be sufficient for prevention of fatty liver.[13] The risk of choline deficiency is higher in men, postmenopausal women, and vegans or vegetarians.
|
Life Stage |
Age | Males | Females |
|
Children |
9-13 years |
375 |
375 |
|
Adolescents |
14-18 years |
550 |
400 |
| Adults | 19 years and older | 550 |
425 |
| Breast-feeding |
550 |
Adequate Intake (AI) for Choline (mg/d), Linus Pauling Institute Micronutrient Information Center
Many botanicals have hepatoprotective (liver protective) action and may further reduce the risk of NAFLD and NASH.[14] Turmeric (Curcuma longa) and its active constituents (curcuminoids) serve as antioxidants and are very effective at reducing inflammation throughout the body, including the liver.[15],[16] Curcumin also has been shown to significantly improve blood levels of triglycerides and LDL-cholesterol, which often are elevated in conjunction with metabolic syndrome and contribute to liver inflammation and fat accumulation.[17] Obesity is often associated with a chronic, low grade, inflammatory state, and curcumin has been shown to lower inflammatory markers such as C-reactive protein (CRP), which also is factor contributing to cardiovascular disease.[18]
Silymarin, a mixture of the active constituents of milk thistle, functions as an antioxidant and has been shown to reduce liver injury caused by acetaminophen, alcohol, iron overload, radiation, consumption of the poisonous mushroom Amanita phalloides (death cap), and other injurious substances.
Milk thistle (Silybum marianum) is an herb best known for its potential hepatoprotective effects. Silymarin, a mixture of the active constituents of milk thistle, functions as an antioxidant and has been shown to reduce liver injury caused by acetaminophen, alcohol, iron overload, radiation, consumption of the poisonous mushroom Amanita phalloides (death cap), and other injurious substances.[19] Beneficial effects of silymarin have been reported in studies of alcoholic liver disease, fatty liver disease, acute and chronic viral hepatitis, and toxin-induced liver diseases.[20],[21],[22]
A variety of foods also support the liver and gallbladder function. This includes dandelion greens, artichokes,[23] beets,[24] parsley,[25] lemon,[26] and burdock.[27] Dandelion (Taraxacum officinale) is used by herbalists to support the liver, gallbladder, and digestive health. Dandelion extracts have been shown to help protect the liver from alcohol- or high-fat diet-induced stress.[28],[29] Dandelion can be consumed in teas, and even as cooked or raw salad greens, however the safety of the source should be considered – don’t pick dandelion greens from a yard that’s been sprayed with pesticides!
Perhaps not surprisingly, probiotics have also been studied for their ability to reduce liver inflammation and related conditions such as hepatic encephalopathy (neurological and psychological problems caused by liver disease). Liver enzyme elevation sometimes accompanies small intestinal bacterial overgrowth (SIBO), celiac disease, increased intestinal permeability, and other gastrointestinal conditions.[30],[31] For this reason, if these conditions are suspected, they should be addressed as part of a comprehensive treatment plan.
Summary
Fortunately, we do not need to wait for Big Pharma to develop a new drug as many of these supplement ingredients have been shown to do just what they are looking for: help reduce the risk of liver damage due to diet or lifestyle. Evidence supports a role for antioxidants (glutathione, N-acetylcysteine, lipoic acid, vitamins C and E), phosphatidylcholine, certain botanical extracts (curcumin, silymarin), and probiotics in the maintenance of liver health. Combined with weight loss and the management of insulin resistance where indicated, the implementation of nutritional strategies may help support not only liver health, but the health of the body systemically.
Click here to see References
[1] Review Team, LaBrecque DR, et al. World Gastroenterology Organisation global guidelines: nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. J Clin Gastroenterol. 2014;48:467-73.
[2] Lazo M, et al. Prevalence of nonalcoholic fatty liver disease in the United States: the Third National Health and Nutrition Examination Survey, 1988-1994. Am J Epidemiol. 2013;178(1):38-45.
[3] Berardis S, Sokal E. Pediatric non-alcoholic fatty liver disease: an increasing public health issue. Eur J Pediatr. 2014 Feb;173(2):131-9.
[4] Ahmed A, et al. Nonalcoholic fatty liver disease review: diagnosis, treatment, and outcomes. Clin Gastroenterol Hepatol. 2015;13:2062-70.
[5] Chen G, et al. Micronutrient antioxidants and nonalcoholic fatty liver disease. Int J Mol Sci. 2016 Aug;17(9).
[6] Mehta K, et al. Nonalcoholic fatty liver disease: pathogenesis and the role of antioxidants. Nutr Rev. 2002 Sep;60(9):289-93.
[7] Yuan L, Kaplowitz N. Glutathione in liver diseases and hepatotoxicity. Mol Aspects Med. 2009 Feb-Apr;30(1-2):29-41.
[8] Ali MH, et al. Protective effect of ursodeoxycholic acid, resveratrol, and N-acetylcysteine on nonalcoholic fatty liver disease in rats. Pharm Biol. 2015 Jul 1:1-11.
[9] Bustamante J, et al. Alpha-lipoic acid in liver metabolism and disease. Free Radic Biol Med. 1998 Apr;24(6):1023-39.
[10] Singh U, et al. Vitamin E, oxidative stress, and inflammation. Annu Rev Nutr. 2005;25:151-74.
[11] Ma X, et al. Polyenylphosphatidylcholine attenuates non-alcoholic hepatic fibrosis and accelerates its regression. J Hepatol. 1996 May;24(5):604-13.
[12] Lieber CS, et al. Phosphatidylcholine protects against fibrosis and cirrhosis in the baboon. Gastroenterology. 1994 Jan;106(1):152-9.
[13] Fischer LM, et al. Sex and menopausal status influence human dietary requirements for the nutrient choline. Am J Clin Nutr. 2007 May;85(5):1275-85.
[14] Jadeja R, et al. Herbal medicines for the treatment of nonalcoholic steatohepatitis: current scenario and future prospects. Evid Based Complement Alternat Med. 2014:648308.
[15] Reyes-Gordillo K, et al. Curcumin protects against acute liver damage in the rat by inhibiting NF-kappaB, proinflammatory cytokines production and oxidative stress. Biochim Biophys Acta. 2007 Jun;1770(6):989-96.
[16] Miyakoshi M, et al. Hepatoprotective effect of sesquiterpenes in turmeric. Biofactors. 2004;21(1-4):167-70.
[17] Shin SK, et al. Long-term curcumin administration protects against atherosclerosis via hepatic regulation of lipoprotein cholesterol metabolism. Mol Nutr Food Res. 2011 Dec;55(12):1829-40.
[18] Sahebkar A. Are curcuminoids effective C-reactive protein-lowering agents in clinical practice? Evidence from a meta-analysis. Phytother Res. 2014 May;28(5):633-42.
[19] Abenavoli L, et al. Milk thistle in liver diseases: past, present, future. Phytother Res. 2010 Oct;24(10):1423-32.
[20] Xiao J, et al. Recent advances in the herbal treatment of non-alcoholic Fatty liver disease. J Tradit Complement Med. 2013 Apr;3(2):88-94.
[21] Malaguarnera M, et al. Silybin-vitamin E-phospholipids complex reduces liver fibrosis in patients with chronic hepatitis C treated with pegylated interferon α and ribavirin. Am J Transl Res. 2015 Nov 15;7(11):2510-8.
[22] Flora K, et al. Milk thistle (Silybum marianum) for the therapy of liver disease. Am J Gastroenterol. 1998 Feb;93(2):139-43.
[23] Rangboo V, et al. The effect of artichoke leaf extract on alanine aminotransferase and aspartate aminotransferase in the patients with nonalcoholic steatohepatitis. Int J Hepatol. 2016;2016:4030476.
[24] Agarwal M, et al. Hepatoprotective activity of Beta vulgaris against CCl4-induced hepatic injury in rats. Fitoterapia. 2006 Feb;77(2):91-3.
[25] Bolkent S, et al. Effects of parsley (Petroselinum crispum) on the liver of diabetic rats: a morphological and biochemical study. Phytother Res. 2004 Dec;18(12):996-9.
[26] Bhavsar SK, et al. Investigation into hepatoprotective activity of Citrus limon. Pharmaceutical Biology. 2007 Jan 1;45(4):303-11.
[27] Predes FS, et al. Antioxidative and in vitro antiproliferative activity of Arctium lappa root extracts. BMC Complement Altern Med. 2011 Mar 23;11:25.
[28] You Y, et al. In vitro and in vivo hepatoprotective effects of the aqueous extract from Taraxacum officinale (dandelion) root against alcohol-induced oxidative stress. Food Chem Toxicol. 2010 Jun;48(6):1632-7.
[29] Davaatseren M, et al. Taraxacum official (dandelion) leaf extract alleviates high-fat diet-induced nonalcoholic fatty liver. Food Chem Toxicol. 2013 Aug;58:30-6.
[30] Ilan Y. Leaky gut and the liver: a role for bacterial translocation in nonalcoholic steatohepatitis. World J Gastroenterol. 2012 Jun 7;18(21):2609-18.
[31] Li DY, et al. Nonalcoholic fatty liver disease: for better or worse, blame the gut microbiota? JPEN J Parenter Enteral Nutr. 2013 Nov;37(6):787-93.
The information provided is for educational purposes only. Consult your physician or healthcare provider if you have specific questions before instituting any changes in your daily lifestyle including changes in diet, exercise, and supplement use.
Share this post
Dr. Carrie Decker
Related posts
CoQ10 vs Astaxanthin
Two Powerhouse Nutrients for Optimal Athletic Performance When it comes to introducing these two powerhouse nutrients, most people have heard of coenzyme Q10 (CoQ10). It has a great reputation as a powerful antioxidant and has been well researched as a cardioprotective nutrient.[1],[2] It has been shown to have a positive impact on blood lipid…
Go Greens, Go Greens, Rah Rah Rah!
Why fruits, berries, and veggies should be a staple in any diet “Crackers and cheese, that’s about all he eats,” a mom tells me when I ask her about her child’s eating habits. “Hm, I see. Any vegetables?” “Only if I put them in the blender and sneak them into tomato sauce.” We both…
Say Yes to NO: Nitric Oxide
Support for heart health, sexual performance, and beyond Nitric oxide (NO) is a tiny gas molecule produced in the blood vessels, nerves, and immune cells. Best known for its role in maintaining blood pressure, NO also mediates penile erections, supports healthy blood flow to the brain, enhances muscle oxygen use during exercise, and helps…
Turmeric: A Golden Remedy for Musculoskeletal Health
Curcuminoids, the famous active compounds from turmeric, deliver benefits for joint health and exercise recovery Liquid gold. Golden milk. That brilliant saffron-hued spice. We hear a lot about turmeric these days—also known as Curcuma longa—a member of the ginger family, and native of Southeast Asia.[1] Valued for its brilliant hue and distinctive spicy-bitter flavor,…
Is Fish Oil Just Snake Oil?
The research on essential fatty acids Some major news channels have reported that fish oil’s importance in heart health has been debunked and that essential fatty acid (EFA) supplements are useless. These types of sensationalist headlines are unhelpful for many reasons, mainly because, well, they’re wrong. It’s been known for many decades just how…
Missing Out on the Keto Craze?
Should you hop on the bandwagon? One of the latest diet trends is the “keto” (ketogenic) diet, which has eclipsed Paleo as the hottest diet trend around. Keto diets are touted as helping you lose weight, improve your memory, and live longer. And a slew of businesses are lining up to capitalize on the…
Categories
- Botanicals (56)
- GI Health (53)
- Healthy Aging (121)
- Immune Support (39)
- In The News (39)
- Kids Health (21)
- Stress and Relaxation (50)
- Uncategorized (1)
- Video (9)
- Vitamins & Minerals (51)